Free Advance Beneficiary Notice of Non-coverage PDF Form
Misconceptions
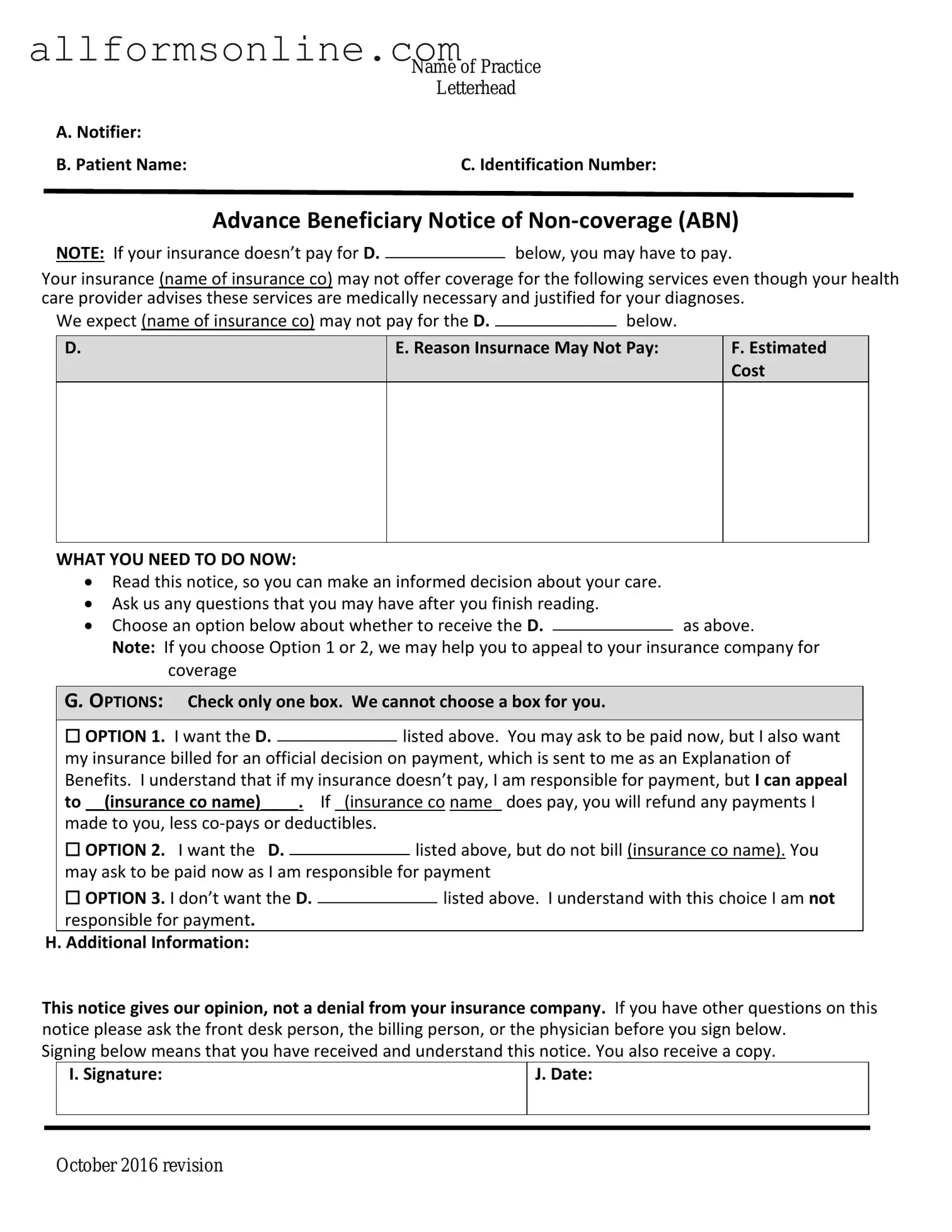
The Advance Beneficiary Notice of Non-coverage (ABN) is an important document that informs Medicare beneficiaries about services that may not be covered. However, several misconceptions surround this form. Below is a list of ten common misunderstandings.
- The ABN is only for Medicare patients. Many believe the ABN applies solely to Medicare beneficiaries. In reality, it can also be used by other insurance providers, depending on their policies.
- Receiving an ABN means the service will not be covered. An ABN indicates that a service may not be covered, but it does not guarantee that coverage will be denied. It is a precautionary measure.
- You must sign the ABN to receive care. Signing the ABN is not a requirement to receive care. Patients can still receive services even if they choose not to sign.
- The ABN is the same as a waiver of liability. While both documents inform patients about potential costs, an ABN specifically addresses non-coverage issues, whereas a waiver of liability relates to liability for care provided.
- All healthcare providers use the ABN. Not all providers utilize the ABN. Some may have different procedures for notifying patients about non-covered services.
- The ABN is only relevant for outpatient services. This form can apply to both outpatient and inpatient services, depending on the situation and the specific services rendered.
- Signing an ABN means you will definitely be billed. Signing the ABN indicates awareness of potential non-coverage, but it does not automatically mean that the patient will incur charges.
- The ABN must be issued before every service. The ABN should be issued when there is a reasonable expectation that a service may not be covered, but it is not necessary for every single service.
- Patients can ignore the ABN. Ignoring the ABN can lead to unexpected costs. Patients should review it carefully and understand their options.
- The ABN is only for elective procedures. The ABN can be issued for both elective and necessary procedures if there is uncertainty about coverage.
Understanding these misconceptions can help beneficiaries make informed decisions about their healthcare and financial responsibilities. Awareness of the ABN's purpose and implications is essential for navigating Medicare services effectively.
What to Know About This Form
What is the Advance Beneficiary Notice of Non-coverage (ABN)?
The Advance Beneficiary Notice of Non-coverage (ABN) is a form that healthcare providers use to inform Medicare beneficiaries that a particular service or item may not be covered by Medicare. It is designed to help patients understand their financial responsibilities before receiving care. If you receive an ABN, it means your provider believes that Medicare may deny payment for the service, and you may be responsible for the costs.
When should I receive an ABN?
You should receive an ABN before you undergo a service or procedure that your healthcare provider thinks Medicare might not cover. This typically happens when the provider believes the service is not medically necessary or when a service is considered experimental. It’s essential to carefully read the ABN, as it outlines your options and what you can expect regarding payment.
What should I do if I receive an ABN?
Can I appeal if Medicare denies coverage after I received an ABN?
Yes, you can appeal a Medicare denial even after receiving an ABN. If Medicare denies coverage for the service listed on the ABN, you have the right to request a review of the decision. The appeal process typically involves submitting a written request to Medicare, explaining why you believe the service should be covered. Make sure to keep copies of all documentation, including the ABN, as it will be essential during the appeal process.
Different PDF Forms
Simple Owner Operator Lease Agreement - Owner Operator must provide written receipts for goods received from the Carrier.
To ensure the confidentiality of sensitive information, parties may consider utilizing a comprehensive Non-disclosure Agreement document that details their obligations and protections. This critical legal instrument serves to secure proprietary knowledge, fostering collaboration while minimizing the risk of unauthorized disclosure. For more information and to access the form, please visit the resource on Non-disclosure Agreement requirements.
96 Well Plate Map - Each well can hold a specific volume of liquid, often 100-200 µL.
Cg2010 Additional Insured Endorsement - Liability does not extend to scenarios beyond the defined ongoing operations for additional insureds.
How to Use Advance Beneficiary Notice of Non-coverage
After receiving the Advance Beneficiary Notice of Non-coverage form, the next steps involve carefully completing the required fields to ensure accurate processing. This form is crucial for documenting that certain services may not be covered by Medicare. Follow the instructions below to fill out the form correctly.
- Begin by entering the date at the top of the form. This should be the date you are filling out the form.
- Next, provide the patient’s name in the designated space. Ensure that the name matches the one on the Medicare card.
- Fill in the patient’s Medicare number. This number is typically found on the Medicare card.
- Indicate the specific service or item that is being discussed. Be clear and concise in your description.
- In the next section, explain why the service may not be covered. Use straightforward language to outline the reasons.
- After that, include the name and signature of the provider who is issuing the notice. This confirms that the provider has communicated the potential non-coverage to the patient.
- Lastly, provide the date of the provider's signature. This should match the date the notice was given to the patient.