Free Annual Physical Examination PDF Form
Misconceptions
Understanding the Annual Physical Examination form is essential for ensuring a smooth and efficient medical appointment. However, several misconceptions can lead to confusion. Here are four common misunderstandings about the form:
- Misconception 1: The form is optional.
- Misconception 2: All sections must be filled out in detail.
- Misconception 3: The form only concerns physical health.
- Misconception 4: You can complete the form during the appointment.
Some people believe that completing the Annual Physical Examination form is optional. In reality, it is crucial to fill out the form entirely before the appointment. This information helps healthcare providers understand your medical history and current health status, which can lead to more accurate assessments and recommendations.
While it is important to provide as much information as possible, not every section requires exhaustive details. For instance, if you have no allergies or chronic conditions, you can simply indicate that. Focus on providing relevant and accurate information rather than stressing over every blank space.
Many assume the form is solely about physical health, but it encompasses a broader scope. It includes mental health considerations, medication lists, and lifestyle factors. Addressing these areas allows healthcare providers to offer comprehensive care tailored to your needs.
Some individuals think they can fill out the form while waiting for their appointment. However, it is best to complete it beforehand to avoid delays. Taking the time to gather your medical history and medications before arriving ensures a more efficient visit.
What to Know About This Form
What is the purpose of the Annual Physical Examination form?
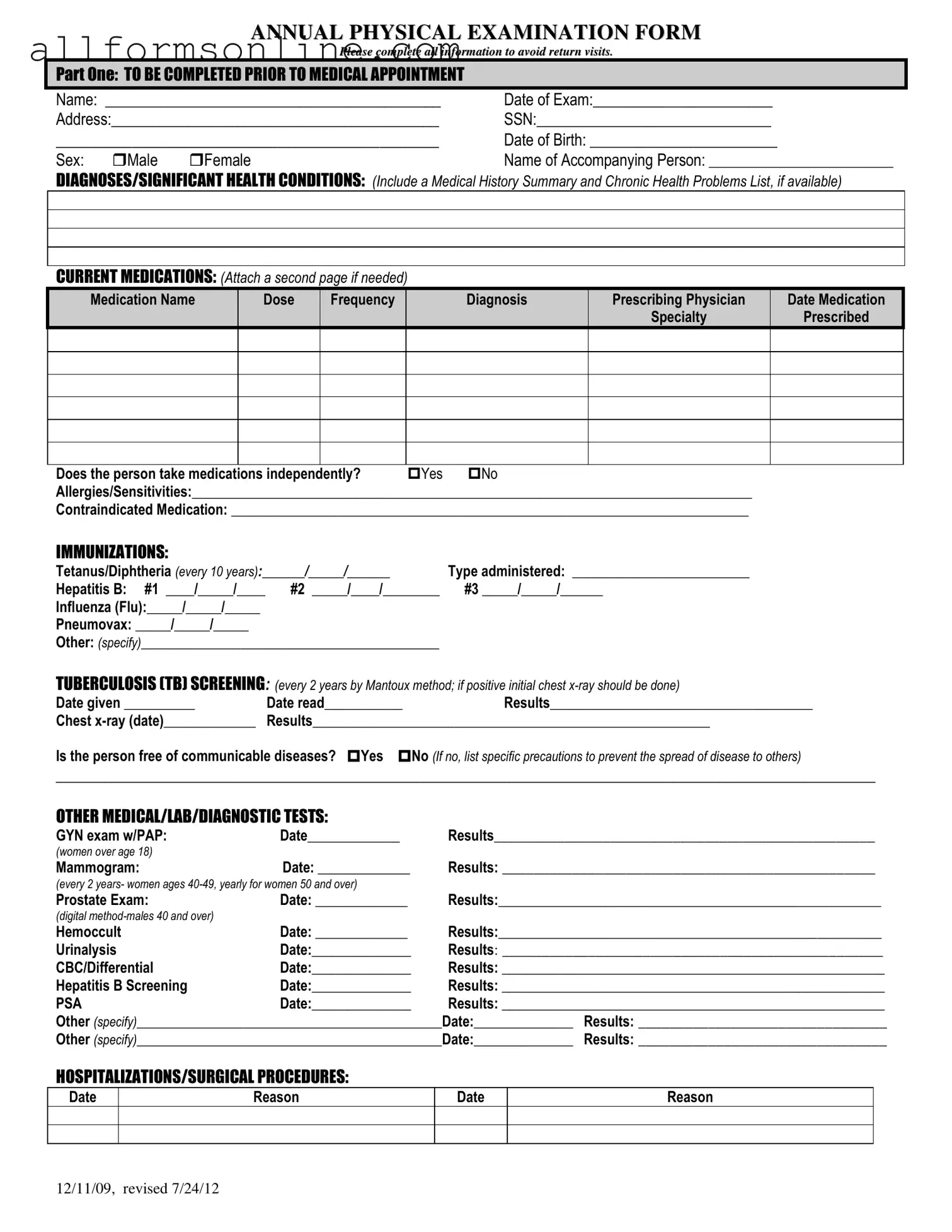
The Annual Physical Examination form is designed to gather important health information about an individual before their medical appointment. It helps ensure that the healthcare provider has a comprehensive understanding of the patient's medical history, current medications, allergies, and any significant health conditions. Completing this form accurately can help avoid the need for return visits due to missing information.
What information is required in Part One of the form?
Part One of the form requires personal details such as the individual's name, date of exam, address, Social Security number, date of birth, and sex. It also asks for the name of an accompanying person and details about any significant health conditions, current medications, allergies, and immunizations. This section aims to provide a complete picture of the individual's health status prior to the appointment.
How should medications be listed on the form?
When listing medications, include the name of each medication, the dose, frequency of intake, diagnosis for which it is prescribed, the name of the prescribing physician, and the date it was prescribed. If there are multiple medications, attach an additional page as needed. Indicate whether the person takes medications independently and note any allergies or sensitivities to medications.
What is included in Part Two of the form?
Part Two of the form focuses on the general physical examination. It includes vital signs such as blood pressure, pulse, respirations, temperature, height, and weight. It also assesses various body systems, asking whether normal findings were observed. Additional comments can be made regarding medical history, medication changes, recommendations for health maintenance, and any limitations or restrictions on activities.
What should be done if there is a change in health status from the previous year?
If there has been a change in health status, it should be noted on the form. Specify the nature of the change and any relevant details. This information is crucial for the healthcare provider to understand the individual's current health situation and to make informed decisions regarding their care.
Different PDF Forms
Shower Sheets Cna - The form includes sections for recording lesions and decubitus.
When completing the transaction for a motorcycle, it is important to have the right documentation, such as the California Motorcycle Bill of Sale form that you can obtain from Fast PDF Templates. This form ensures that the details of the sale are clearly outlined and safeguards the interests of both the buyer and the seller.
Simple Owner Operator Lease Agreement - There are specific requirements for transporting hazardous materials.
Time Clock Template - The time card assists in accurately calculating payroll for every employee.
How to Use Annual Physical Examination
Completing the Annual Physical Examination form is essential for ensuring that all necessary health information is accurately recorded prior to the medical appointment. Properly filling out the form helps streamline the examination process and avoids the need for additional visits.
- Personal Information: Fill in your name, date of exam, address, Social Security Number (SSN), date of birth, and sex (male or female).
- Accompanying Person: If applicable, provide the name of the person accompanying you to the appointment.
- Medical History: List any diagnoses or significant health conditions. Include a summary of your medical history and any chronic health problems, if available.
- Current Medications: Document all medications you are currently taking, including the medication name, dose, frequency, diagnosis, prescribing physician, and date prescribed. Indicate if you take medications independently and note any allergies or sensitivities.
- Immunizations: Record the dates of any immunizations received, including Tetanus/Diphtheria, Hepatitis B, Influenza, and Pneumovax. Specify any other immunizations.
- Tuberculosis Screening: Enter the date given and date read for TB screening, along with the results and any chest x-ray details if applicable.
- Medical Tests: Provide information about any additional medical, lab, or diagnostic tests completed, including dates and results for GYN exams, mammograms, prostate exams, hemoccult tests, urinalysis, CBC, Hepatitis B screening, and PSA tests.
- Hospitalizations/Surgical Procedures: List any hospitalizations or surgeries with corresponding dates and reasons.
- General Physical Examination: Fill in your blood pressure, pulse, respirations, temperature, height, and weight.
- Evaluation of Systems: For each system listed, indicate whether normal findings were observed and provide comments as necessary.
- Vision and Hearing Screening: Note whether further evaluation is recommended for either vision or hearing.
- Additional Comments: Review your medical history summary and document any medication changes, recommendations for health maintenance, dietary instructions, and any limitations or restrictions for activities.
- Adaptive Equipment: Indicate whether you use any adaptive equipment and specify what it is.
- Change in Health Status: Note if there has been a change in health status from the previous year.
- Physician Information: Print the name of the physician, obtain their signature, and provide the physician's address and phone number.