Free Cna Shower Sheets PDF Form
Misconceptions
Misconceptions about the CNA Shower Sheets form can lead to confusion regarding its purpose and use. Here are four common misunderstandings:
- It is only for reporting severe skin issues. Many believe the form is only necessary for serious conditions like deep wounds or infections. In reality, it is designed for all skin assessments, including minor issues like dryness or bruising.
- Only the charge nurse needs to see the form. Some think that the form is solely for the charge nurse's review. However, it is essential for the Director of Nursing (DON) to also receive any forwarded reports for comprehensive care management.
- Visual assessments are optional. There is a misconception that conducting a visual assessment is not mandatory. In fact, performing this assessment is crucial for identifying any skin abnormalities promptly.
- The form is only for documenting skin problems. While the primary purpose is to document skin conditions, the form also facilitates communication between CNAs, charge nurses, and the DON regarding the resident's overall care needs.
What to Know About This Form
What is the purpose of the CNA Shower Sheets form?
The CNA Shower Sheets form is designed to facilitate a thorough visual assessment of a resident's skin during their shower. This assessment helps identify any abnormalities, such as bruises, rashes, or skin tears. By documenting these findings, the form ensures that any issues are promptly reported to the charge nurse and subsequently reviewed by the Director of Nursing (DON).
What should a CNA do if they notice an abnormality on a resident's skin?
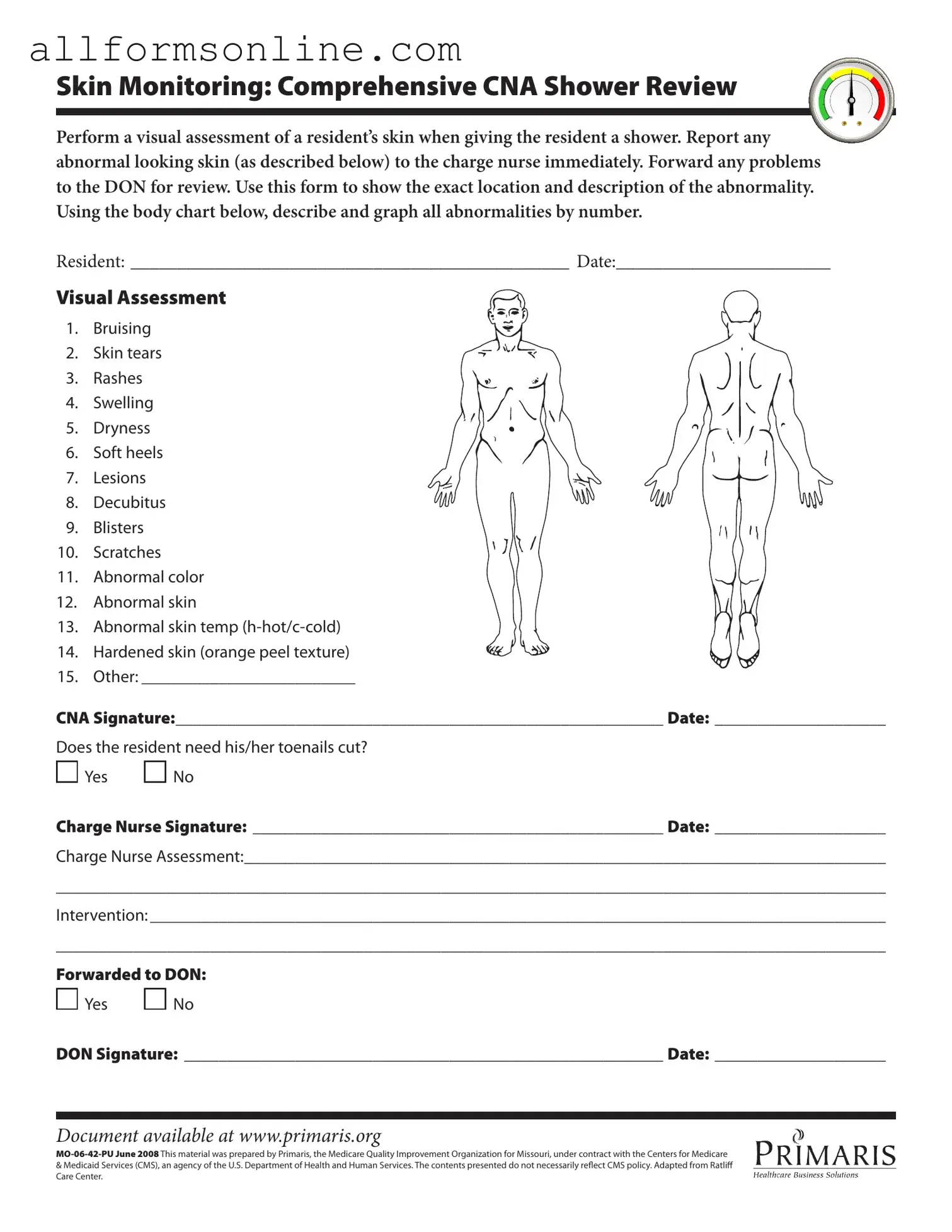
If a CNA observes any abnormal skin conditions while showering a resident, they must report these findings to the charge nurse immediately. It is crucial to provide a detailed description of the abnormality and its exact location using the body chart included in the form. This prompt reporting is essential for ensuring the resident receives appropriate care.
What types of skin abnormalities should be monitored?
The form outlines several specific skin conditions that should be monitored, including bruising, skin tears, rashes, swelling, dryness, and more. Each of these conditions can indicate varying levels of concern and may require different interventions. The form provides a comprehensive list to guide CNAs in their assessments.
How is the information documented on the CNA Shower Sheets form?
Documentation on the CNA Shower Sheets form involves filling out the resident's name, the date, and the specific abnormalities observed. CNAs use the body chart to graphically indicate the locations of these abnormalities. After completing the assessment, the CNA must sign the form, and it may also require signatures from the charge nurse and the DON, depending on the findings.
Is there a section for toenail care on the form?
Yes, the form includes a section that addresses whether the resident needs their toenails cut. This is an important aspect of personal care and can impact the resident's overall health and comfort. The CNA can simply mark "Yes" or "No" in response to this question.
What happens after the CNA completes the form?
Once the CNA completes the form, it should be submitted to the charge nurse for review. The charge nurse will then assess the documented abnormalities and determine any necessary interventions. If needed, the information will be forwarded to the DON for further evaluation and action.
Where can I access the CNA Shower Sheets form?
The CNA Shower Sheets form is available online at www.primaris.org. This resource ensures that CNAs can easily access the form when needed, facilitating consistent and thorough skin assessments for residents.
Different PDF Forms
Acord Form - It can be used for various types of coverage, including liability and property.
Creating a reliable Last Will and Testament document is crucial for individuals looking to clearly define their wishes regarding asset distribution after death. This legal form provides peace of mind, ensuring that your estate is handled according to your preferences while alleviating potential disputes among beneficiaries.
Bill of Lading Form Pdf - This document serves as proof of ownership during transport.
How Do You Set Up Direct Deposit - Direct deposit options with Citibank adapt to fit your lifestyle.
How to Use Cna Shower Sheets
Completing the CNA Shower Sheets form requires careful attention to detail. This form is essential for documenting any skin abnormalities observed during a resident's shower. Following these steps will ensure that all necessary information is accurately recorded, facilitating proper care and follow-up.
- Begin by entering the resident's name in the space labeled RESIDENT.
- Next, fill in the date of the assessment in the DATE field.
- Conduct a visual assessment of the resident's skin during the shower.
- Identify any abnormalities from the list provided, which includes bruising, skin tears, rashes, and more.
- For each abnormality noted, use the body chart to mark its exact location and provide a brief description.
- Sign the form in the CNA Signature section and include the date of the assessment.
- Indicate whether the resident needs their toenails cut by checking either Yes or No.
- Have the charge nurse sign the form in the Charge Nurse Signature section and date it.
- The charge nurse should provide their assessment in the designated area.
- Document any interventions taken in the Intervention section.
- Finally, indicate whether the information has been forwarded to the Director of Nursing (DON) by checking Yes or No.
- Ensure the DON signs the form and includes the date.