Blank Do Not Resuscitate Order Form
Do Not Resuscitate OrderDocuments for Particular States
Misconceptions
Many people have misunderstandings about the Do Not Resuscitate (DNR) Order form. These misconceptions can lead to confusion and stress during critical moments. Here are seven common misconceptions:
- A DNR means I will not receive any medical treatment. This is false. A DNR specifically addresses resuscitation efforts, not all medical care. Patients can still receive other treatments, such as pain relief and comfort care.
- Only terminally ill patients need a DNR. This is not true. Anyone can choose a DNR, regardless of their health status. It is a personal choice based on individual preferences.
- A DNR is only valid in a hospital setting. This misconception is incorrect. A DNR can be valid in various settings, including at home or in nursing facilities, as long as it is properly documented.
- Having a DNR means I will die sooner. This is misleading. A DNR does not hasten death. It simply means that if a person’s heart stops or they stop breathing, they do not want resuscitation efforts.
- I can’t change my mind once I have a DNR. This is false. Individuals can change or revoke their DNR at any time, as long as they communicate their wishes clearly to their healthcare providers.
- All DNR orders are the same. This is not accurate. DNR orders can vary by state and facility. It’s essential to understand the specific requirements and forms applicable to your location.
- Family members can override a DNR order. This is typically incorrect. A DNR order is a legal document that reflects the patient’s wishes. Family members cannot override it unless they have legal authority to make healthcare decisions for the patient.
Understanding these misconceptions can help individuals make informed decisions about their healthcare preferences.
What to Know About This Form
What is a Do Not Resuscitate (DNR) Order?
A Do Not Resuscitate Order is a medical directive that informs healthcare providers not to perform cardiopulmonary resuscitation (CPR) if a patient's heart stops beating or if they stop breathing. This order is typically put in place for individuals who wish to avoid aggressive life-saving measures in the event of a medical emergency.
Who can request a DNR Order?
Generally, a DNR Order can be requested by a patient who is capable of making their own medical decisions. If the patient is unable to communicate their wishes, a legally authorized representative, such as a family member or designated healthcare proxy, may request the order on their behalf.
How is a DNR Order created?
A DNR Order is usually created in consultation with a healthcare provider. The process may involve filling out a specific form that outlines the patient's wishes. It's essential that this form is signed by both the patient (or their representative) and a physician to ensure it is legally valid.
Is a DNR Order valid in all settings?
Yes, a DNR Order is generally valid in all healthcare settings, including hospitals, nursing homes, and at home. However, it is crucial to communicate the existence of the DNR Order to all healthcare providers involved in the patient's care to ensure that their wishes are respected.
Can a DNR Order be revoked?
Absolutely. A patient or their authorized representative can revoke a DNR Order at any time. This can be done verbally or in writing. It’s important to inform healthcare providers immediately if the order is revoked to avoid any confusion during a medical emergency.
What happens if a DNR Order is not in place?
If a DNR Order is not in place and a patient experiences cardiac arrest or respiratory failure, healthcare providers will typically initiate CPR and other life-saving measures. This may include chest compressions, intubation, and medications, depending on the situation and the patient's condition.
How does a DNR Order differ from other advance directives?
A DNR Order specifically addresses the issue of resuscitation, while other advance directives, such as living wills or healthcare proxies, may cover a broader range of medical decisions. Living wills outline a person's preferences for medical treatment in various situations, while healthcare proxies designate someone to make decisions on the patient's behalf when they are unable to do so.
Will a DNR Order affect other medical treatments?
No, a DNR Order only applies to resuscitation efforts. It does not affect other medical treatments or interventions. Patients with a DNR Order can still receive medications, pain management, and other necessary care, as well as comfort measures to ensure their quality of life.
How can I ensure my DNR Order is honored?
To ensure your DNR Order is honored, it is important to communicate your wishes clearly to your healthcare providers and family members. Keep a copy of the DNR Order in an accessible place, such as your medical records, and consider wearing a medical alert bracelet that indicates your DNR status.
Where can I obtain a DNR Order form?
DNR Order forms can often be obtained from your healthcare provider, hospital, or state health department. Some states also provide downloadable forms on their official websites. Make sure to use the correct form for your state, as requirements may vary.
Popular Templates:
Do Golf Carts Have a Title - This document can be customized to include specific terms negotiated by the parties.
In addition to understanding the application process, it is essential to utilize reliable resources for completing the EDD DE 2501 form, such as the templates offered by Fast PDF Templates, which can help streamline the submission and ensure all required information is included for a successful claim.
Ucc 1308 - This document is available to anyone wishing to reserve their rights proactively.
How to Use Do Not Resuscitate Order
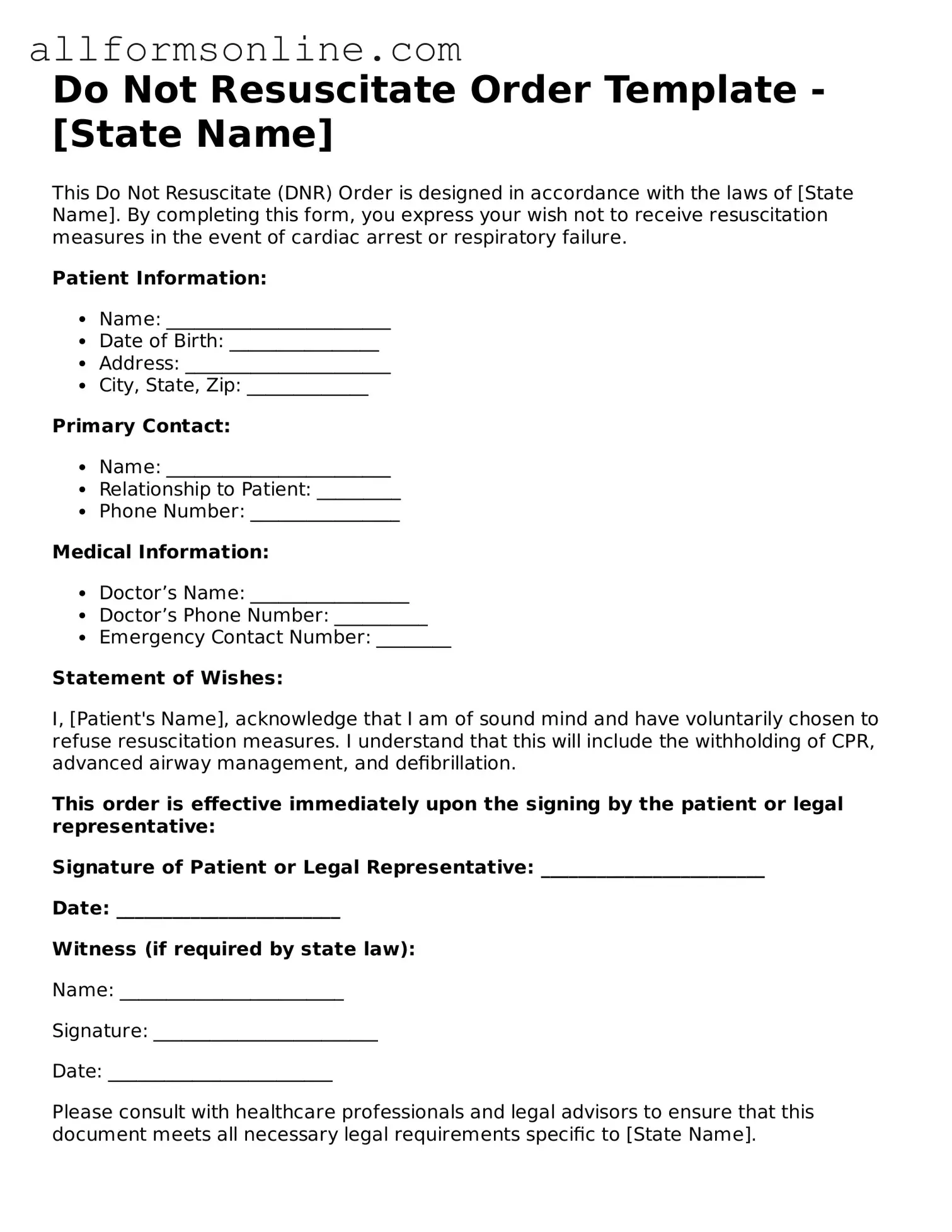
When preparing to fill out the Do Not Resuscitate Order (DNR) form, it’s essential to ensure that all necessary information is accurately provided. This form allows individuals to express their wishes regarding medical interventions in the event of a life-threatening situation. Follow these steps carefully to complete the form effectively.
- Start by entering your full name at the top of the form.
- Provide your date of birth. This helps to confirm your identity.
- Include your address. Make sure it is current to avoid any confusion.
- Indicate the name of your healthcare provider or physician. This is important for medical records.
- Sign the form. Your signature shows that you understand and agree to the contents of the form.
- Date the form. This helps to establish when the order was made.
- Have a witness sign the form if required. Some states may require a witness for validity.
- Make copies of the completed form for your records and to share with your healthcare provider.
After you have filled out the form, keep it in a safe but accessible place. It’s important that your loved ones and healthcare providers are aware of your wishes, so consider discussing your decision with them. This ensures everyone is on the same page when it comes to your healthcare preferences.