Free Medication Administration Record Sheet PDF Form
Misconceptions
Understanding the Medication Administration Record (MAR) Sheet is crucial for ensuring proper medication management. However, several misconceptions exist regarding its use and purpose. Here are ten common misconceptions:
- The MAR sheet is only for nurses. Many believe only nurses can use the MAR sheet, but it is a tool for all healthcare providers involved in medication administration.
- It is optional to complete the MAR sheet. Some think that filling out the MAR sheet is optional, but accurate documentation is essential for patient safety and legal compliance.
- One entry per day is sufficient. Many assume that one entry for the entire day is enough. In reality, each medication administration must be recorded at the time it occurs.
- All medications are listed on the MAR sheet. Some people believe that all medications a patient takes will appear on the MAR sheet. However, it only includes medications prescribed for the specific time frame covered by the sheet.
- Refused medications do not need to be documented. There is a misconception that refused medications do not require documentation. In fact, any refusal must be noted to ensure proper follow-up.
- MAR sheets are only for in-patient settings. Some think that MAR sheets are only used in hospitals. They are also essential in outpatient settings, assisted living facilities, and home care.
- Changes in medication do not need to be recorded immediately. Many believe they can wait to record changes in medication. However, timely updates are critical for maintaining accurate records.
- Initials can replace full names on the MAR sheet. Some assume that using initials is sufficient. Full names are necessary to avoid any confusion regarding medication administration.
- All errors in documentation can be corrected without consequence. It is a common belief that mistakes can be erased or altered freely. However, proper protocols must be followed to correct errors to maintain the integrity of the record.
- Once completed, the MAR sheet does not need to be reviewed. Some think that after filling out the MAR sheet, it is no longer necessary to review it. Regular audits are important for ensuring compliance and accuracy.
By addressing these misconceptions, healthcare providers can improve their understanding of the MAR sheet and enhance patient care.
What to Know About This Form
What is the purpose of the Medication Administration Record Sheet?
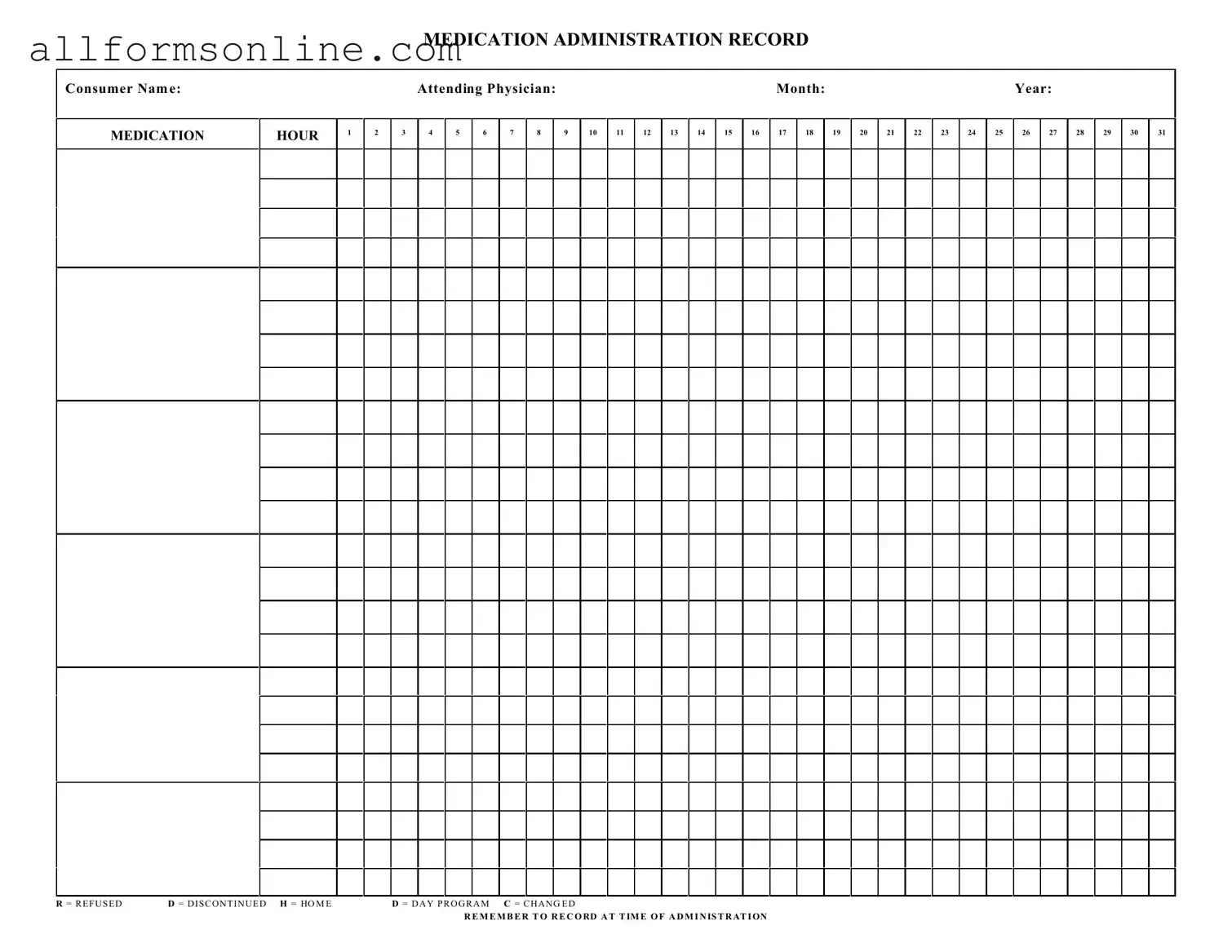
The Medication Administration Record Sheet (MARS) is a crucial tool used to track the administration of medications to consumers. It ensures that each dose is documented accurately, helping caregivers and healthcare professionals monitor medication schedules and adherence. This record is essential for maintaining the health and safety of individuals receiving medications.
How should I fill out the Medication Administration Record Sheet?
When filling out the MARS, start by entering the consumer's name, the attending physician's name, and the month and year. Each medication should be listed along with the corresponding time it is to be administered. As you administer the medication, mark the appropriate box for each hour. If a dose is refused, discontinued, or changed, use the designated letters (R, D, C) to indicate these actions clearly. Remember to document at the time of administration to ensure accuracy.
What do the abbreviations on the form mean?
The MARS includes several abbreviations to indicate specific actions or statuses. "R" stands for "Refused," meaning the consumer did not take the medication. "D" indicates "Discontinued," which shows that the medication is no longer being administered. "H" refers to "Home," indicating the consumer is at home rather than in a facility. "D" for "Day Program" signifies that the consumer is participating in a day program, and "C" means "Changed," which notes any alterations in the medication regimen. Understanding these abbreviations is vital for accurate record-keeping.
Why is it important to record medication administration at the time it occurs?
Recording medication administration at the time it occurs is crucial for several reasons. It helps prevent errors by ensuring that the information is fresh in the caregiver's mind. Timely documentation also provides an accurate account of what medications have been given, which is essential for tracking the consumer's health and response to treatment. This practice can significantly reduce the risk of missed doses or incorrect administration, ultimately enhancing patient safety.
What should I do if I make a mistake on the Medication Administration Record Sheet?
If you make a mistake on the MARS, do not attempt to erase it. Instead, draw a single line through the error and initial it. Then, write the correct information next to it. This method maintains a clear record of what occurred, ensuring transparency and accountability in medication administration. Keeping accurate records is vital for the consumer's health and the integrity of the healthcare process.
Who is responsible for maintaining the Medication Administration Record Sheet?
Typically, the responsibility for maintaining the MARS falls on the healthcare professionals and caregivers directly involved in administering medications. This includes nurses, nursing assistants, and other staff members trained in medication administration. However, it is a shared responsibility, and everyone involved in the consumer's care should ensure that the records are accurate and up-to-date. Regular audits may also be conducted to ensure compliance with documentation standards.
Different PDF Forms
USCIS Form I-864 - Sponsors must meet or exceed 125% of the federal poverty guidelines to qualify.
For those looking to make the vehicle purchasing process clearer, utilizing templates such as the Fast PDF Templates can be incredibly beneficial. These templates help simplify the completion of essential paperwork, ensuring that buyers and sellers can easily navigate through the specific terms and conditions outlined in the California Vehicle Purchase Agreement.
Odometer Disclosure Statement Ca - This statement ensures that all parties involved have mutually agreed upon the vehicle's mileage at the time of sale.
5e Fillable Character Sheet - Capture your character's aspirations and dreams for the future.
How to Use Medication Administration Record Sheet
Completing the Medication Administration Record Sheet is essential for accurately tracking medication administration for consumers. Following the steps outlined below will help ensure that the form is filled out correctly and comprehensively.
- Begin by entering the Consumer Name at the top of the form.
- Next, provide the name of the Attending Physician in the designated space.
- Fill in the Month and Year in the appropriate fields.
- In the section labeled MEDICATION, list each medication that needs to be administered.
- For each medication, mark the HOUR when it is to be administered, from 1 to 24.
- As medications are administered, record the date in the corresponding boxes for each hour.
- If a medication is refused, use the letter R in the appropriate box. If it has been discontinued, use D. For medications given at home, use H, and for those given at a day program, use D again. If there is a change, indicate this with C.
- Remember to record the time of administration accurately for each entry.